Pastoral Care Team Training Presentation Notes
What is Congregational Pastoral Care and How has it Changed since the Pandemic?
Elizabeth Chown Lafrenière, Coordinator, Family Life Centre Oct 24, 2023
Congregational Pastoral Care is a gift. It is a gift to receive, to know that we are cared for and supported and not forgotten. It is a gift that reaffirms our faith, and reassures us that God’s love accompanies us at all times, in all ways. It is a gift when God sends a friend or a Congregational Pastoral Care Team member to listen, to hold space with us and to walk with us, literally and figuratively. Congregational Pastoral Care is a gift to the giver as well. It is a gift that strengthens our faith.
A Pastoral Care Team is a group of caring people who assist and support the lead minister by listening, praying and offering practical support. Pastoral Care Team does not:
Everything the volunteer does is as a Pastoral Care Team member on behalf of the Minister and congregation. This avoids an unhealthy reliance or dependency, or feelings of being beholden to an individual, or burnout by the Team member.
Pastoral Care involves listening deeply; listening for what the person feels comfortable sharing. You don't know what baggage someone bring to the conversation. Their reaction to an acute event may include chronic issues so tread lightly.
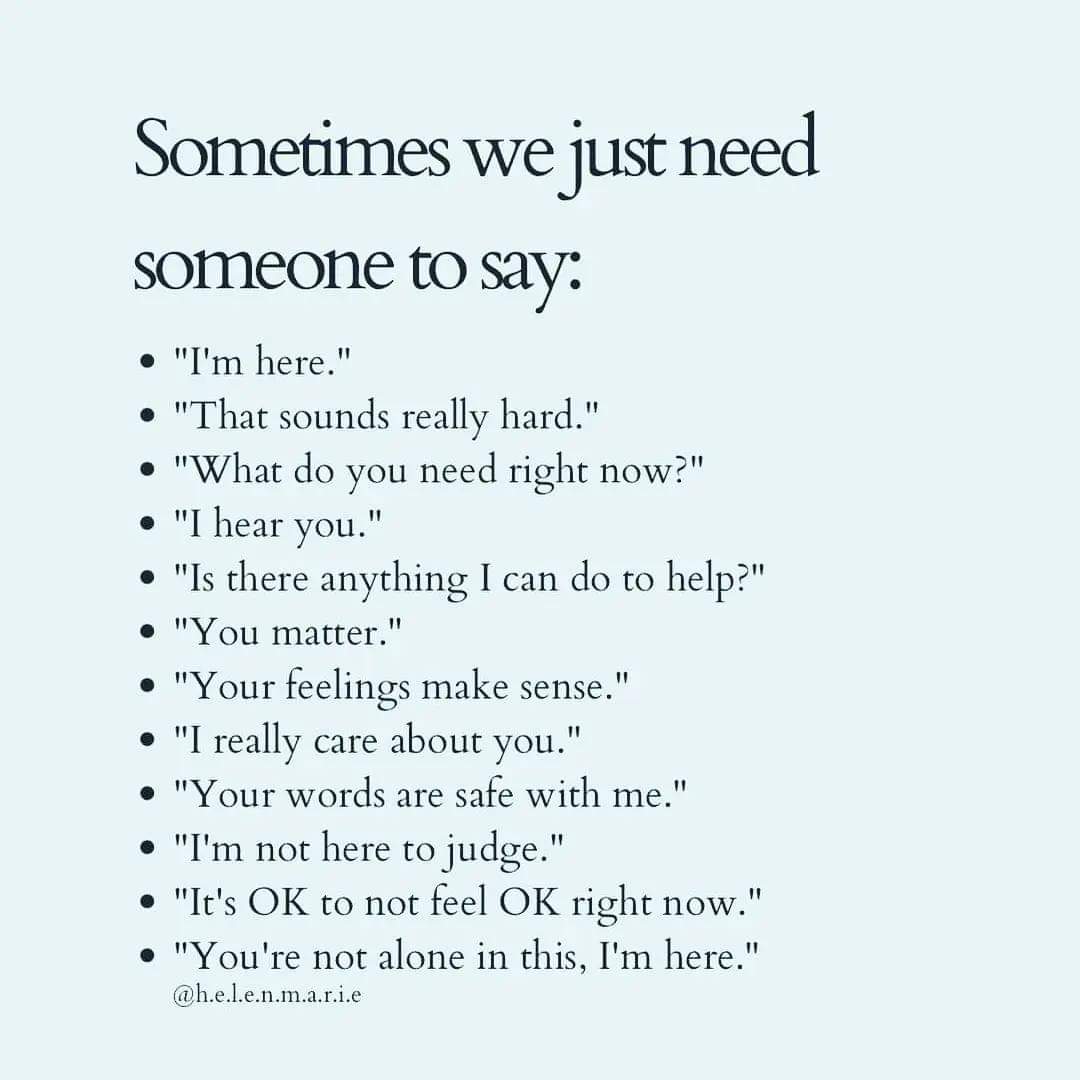
Pastoral Care is being there, in a way the receiver finds helpful. It’s holding space with someone in a time of need. It's listening without judgement, without problem-solving, without breaching confidentiality.
It's fulfilling practical needs -- where possible -- in ways that support the person seeking care, without creating an imbalance.
Practice the Pause. You want to create a safe space for this person to express their feelings, fear, frustrations and hopes.
Since the pandemic, we all aged more than 3 years. Feelings of vulnerability and mortality increased, we lost friends and didn’t have the traditional rites of passage and collective grieving. We realized we know people experiencing food insecurity and economic stress in these inflationary times. Many people downsized, moving to assisted living. Some express more concerns of what will happen with their special needs adult child. We now know more about triggers, and privilege, and mental health crises.
In post-pandemic Pastoral Care, what used to be done face-to-face is now done by phone, at least initially, without visual cues.
Before any call or visit
Hospital visits should be brief – 15 minutes is fine.
Home visit = the time it takes to make and drink a cup of tea; about 45 minutes.
Visiting someone in palliative care is a very special case. Take your lead from the person who is dying. They might tire easily or they might have a lot to say. Prepare yourself that they may want to talk about dying, they may be angry, they may be sad, they may want to discuss current events or politics or gardening tips, or they may want to reminisce. If you have shared memories, reliving those moments together can be a lovely gift, and remember, it's okay for you both to laugh.
After the call or visit:
Respect boundaries. Maintain confidentiality. It’s their story. It’s their news. It’s their life, and it’s not your place to usurp what could be the only sense of control they have in this moment.
Remember: it’s okay to say “I don’t know what to say.”
Some helpful words and phrases
I've brought a few cookies to share. Could we put the kettle on together for a cup of tea?
We don't know each other well but I would really like to offer you some support. I am a good listener if you feel like talking.
Thank you for sharing.
Thank you for trusting me with that.
I appreciate that you shared that with me.
I am touched by what you've shared with me.
Instead of How are you? Try these:
How is today going?
You've been in my mind.
I'm glad to be here with you.
I've been thinking about you.
How are you feeling?
How are you, really?
Should I ask how you are or not?
What's going well today and what's not?
Who do you need to call -- are they any calls I could initiate for you?
I am happy to listen, if it would help to talk.
I can just be here to keep you company, we don't need to talk if you're not feeling up to it.
What would be helpful right now?
When did you eat? Could I bring something?
Could I help you with the children's supper?
I will pray for you. Would you like me to pray with you right here, right now?
Tell me some stories about him/her.
Never say 'you're so strong'. A more caring way to acknowledge the caregiver is “I'm concerned about you. Are you getting the care you need?”
Elizabeth Chown Lafrenière, Coordinator, Family Life Centre Oct 24, 2023
Congregational Pastoral Care is a gift. It is a gift to receive, to know that we are cared for and supported and not forgotten. It is a gift that reaffirms our faith, and reassures us that God’s love accompanies us at all times, in all ways. It is a gift when God sends a friend or a Congregational Pastoral Care Team member to listen, to hold space with us and to walk with us, literally and figuratively. Congregational Pastoral Care is a gift to the giver as well. It is a gift that strengthens our faith.
A Pastoral Care Team is a group of caring people who assist and support the lead minister by listening, praying and offering practical support. Pastoral Care Team does not:
- offer counseling,
- provide medical advice,
- take on a role that’s best left to someone’s family
Everything the volunteer does is as a Pastoral Care Team member on behalf of the Minister and congregation. This avoids an unhealthy reliance or dependency, or feelings of being beholden to an individual, or burnout by the Team member.
Pastoral Care involves listening deeply; listening for what the person feels comfortable sharing. You don't know what baggage someone bring to the conversation. Their reaction to an acute event may include chronic issues so tread lightly.
Pastoral Care is being there, in a way the receiver finds helpful. It’s holding space with someone in a time of need. It's listening without judgement, without problem-solving, without breaching confidentiality.
It's fulfilling practical needs -- where possible -- in ways that support the person seeking care, without creating an imbalance.
Practice the Pause. You want to create a safe space for this person to express their feelings, fear, frustrations and hopes.
Since the pandemic, we all aged more than 3 years. Feelings of vulnerability and mortality increased, we lost friends and didn’t have the traditional rites of passage and collective grieving. We realized we know people experiencing food insecurity and economic stress in these inflationary times. Many people downsized, moving to assisted living. Some express more concerns of what will happen with their special needs adult child. We now know more about triggers, and privilege, and mental health crises.
In post-pandemic Pastoral Care, what used to be done face-to-face is now done by phone, at least initially, without visual cues.
Before any call or visit
- Make some notes in advance; some words and phrases you’d like to use.
- Familiarize yourself with the person’s circumstances. Know their children’s names, for example. Write them down. Whatever your minister told you when asking you to offer to liaise with this person, review those notes.
- Know your own triggers. Recognize if you have compassion fatigue. It’s okay to decline the minister’s request.
- Understand your goal. In the first call, you want to explain why the minister asked you to call, create trust and open a dialogue. You want to listen.
- Pray. Pray for the person and pray for yourself. Open your mind and heart to listen for the Spirit.
Hospital visits should be brief – 15 minutes is fine.
Home visit = the time it takes to make and drink a cup of tea; about 45 minutes.
Visiting someone in palliative care is a very special case. Take your lead from the person who is dying. They might tire easily or they might have a lot to say. Prepare yourself that they may want to talk about dying, they may be angry, they may be sad, they may want to discuss current events or politics or gardening tips, or they may want to reminisce. If you have shared memories, reliving those moments together can be a lovely gift, and remember, it's okay for you both to laugh.
After the call or visit:
- Write notes when things are fresh in your mind.
- Give yourself time to process how YOU feel.
- Prepare your brief report for the minister, if that’s the process she or he has requested.
- Grieve outwardly, express your pain to someone outside the person’s immediate circle. Do not put the bereaved in the position of consoling you.
- Ask to be relieved if you feel you cannot continue accompanying that care receiver. Your minister doesn’t want two crises created from one and will find someone else to take over, without thinking any less of you.
Respect boundaries. Maintain confidentiality. It’s their story. It’s their news. It’s their life, and it’s not your place to usurp what could be the only sense of control they have in this moment.
Remember: it’s okay to say “I don’t know what to say.”
Some helpful words and phrases
I've brought a few cookies to share. Could we put the kettle on together for a cup of tea?
We don't know each other well but I would really like to offer you some support. I am a good listener if you feel like talking.
Thank you for sharing.
Thank you for trusting me with that.
I appreciate that you shared that with me.
I am touched by what you've shared with me.
Instead of How are you? Try these:
How is today going?
You've been in my mind.
I'm glad to be here with you.
I've been thinking about you.
How are you feeling?
How are you, really?
Should I ask how you are or not?
What's going well today and what's not?
Who do you need to call -- are they any calls I could initiate for you?
I am happy to listen, if it would help to talk.
I can just be here to keep you company, we don't need to talk if you're not feeling up to it.
What would be helpful right now?
When did you eat? Could I bring something?
Could I help you with the children's supper?
I will pray for you. Would you like me to pray with you right here, right now?
Tell me some stories about him/her.
Never say 'you're so strong'. A more caring way to acknowledge the caregiver is “I'm concerned about you. Are you getting the care you need?”
Miscellaneous notes:
Keep an eye on the family caregiver. A verbal acknowledgement could mean the world. Avoid anything that could cause pain or pressure.
Never comment that someone looks exhausted.
Work with your minister to design a simple way for your congregation members to tell the minister about their illness or concerns.
Watch for visitors or regular attendees experiencing a hard time.
Are there tissues handy in your church?
Is there a quiet space available for those who need an escape?
Are the greeters overly exuberant? They might need a reminder to look for hunched shoulders, red eyes, or maybe you want to stand nearby to watch for that. If an out of town son or daughter accompanies someone to church and none of them are smiling, that could be a clue that something’s wrong.
Is someone noticing when regular onsite or online worshippers are missing for several weeks?
Does someone read the Gazette carefully to see if there are obituary notices of grandparents or siblings of your church members?
Is someone tracking death anniversaries to alert the Minister in advance so he/she can send a note?
Using Texting and email for Pastoral Care
Rev. Ellie Hummel, Multidisciplinary Chaplain, Mount Allison University
The main focus of pastoral care, whether in person, by phone, by text, email or social media is to be present and allow room for the Spirit. The person is a child of God.
Use the right tools – and be sure it is something you are comfortable with. Be aware of what is public and what is not.
Young people do not use email, nor do they check voice mail. Seniors often use texting and private messages. Ask the person which platform they prefer to use.
Passive use of social media:
Active use of the various platforms:
Using social media tools to connect with people and build relationship of trust:
In traumatic times, the person does not always feel like talking – it takes too much energy. Be open to further chat when they feel ready.
Be gentle with yourself. You don’t have to do pastoral care electronically if you are not comfortable.
Using texting and private social media messaging platforms are useful for checking in on someone and can reduce loneliness and isolation. Messages don’t have to be long. The person will know you are thinking about them.
Shared experiences:
Additional note shared by a participant after the session:
Comforting the Mourner
Corrie Sirota M.S.W., P.S.W. OTSTCFQ, OPQ
Grief, Loss and Bereavement Specialist - Counseling & Psychotherapy
Clinical Director, Myra's Kids Foundation www.myraskids.ca
[email protected]
Author of "Someone Died...Now What? A Personal and Professional
Perspective on Coping With Grief and Loss" available on amazon.com
There are 72 euphemisms for ‘died’. People are uncomfortable talking about death.
People grieve differently, the stages of grief are not linear, grief will not go away if you ignore it, children definitely grieve, but in different ways, you don’t know exactly how someone feels, there is no shame in seeking counselling.
Death ends a life, not the relationship. Listen, provide support in ways that are relevant to the person, use the name of the person who died, honour the deceased by recognizing death anniversaries, birthdays, etc.
Be aware that there may be complications to the grief and secondary losses such financial impact, where to live, social fall-out, etc.
Click here for Corrie’s TEDx Laval presentation: Loss and Found: Creating New Normals After Someone You Love Dies:
https://youtu.be/PQ27tYEb74Y
And here is a link to her McGill cares webcast: https://www.youtube.com/watch?v=oATZ9cMVGXs
Pastoral Care Challenges as a Giver and as a Receiver
Paul Clarke
Paul Clarke has been a care receiver and a care provider over the years. He shared some personal stories to illustrate pastoral care, including potential pitfalls of good intentions.
When offering pastoral care, it's often very similar to being a good neighbour, part of a caring community,
Understanding Cultural Context in Our New Demographic
Paul Clarke
In 2013 Paul started working at Action Refugiés Montreal, a small NGO that accompanies refugeed people. Their model is empowerment vs charity.
Things to consider when offering pastoral care or caring community friendship to people who have moved from other countries:
Prayer in visiting/care settings
Rev. Dr. Elisabeth Jones, Cedar Park United Church
Prayer is one thing we all need. Because we’re spiritual beings having a human experience. Mortality undoes us.
Ours, or a loved one’s. Illness – physical, mental, catastrophe, unemployment, not enough money, addictions, gender issues… we experience all of these not just in our matter, our cells, our physical assembly, but in our souls, our beings. We know that prayer takes us to holy ground/space. We tread carefully, and consciously. And it’s a hairbreadth line between careful, conscious prayer with and for another, and self-conscious stumbling (or at least feeling that way! But it’s really worth trying to become a person who can pray with and for (not at or about) someone. So I want to say it IS an essential part of the work of a pastoral care team. And it
should never be left to the Minister to do alone.
Because stories are easier to retain in memory. I’m going to make 5 points about this topic, but to frame them within a story, drawn from my experience.
STORY
The first time I was called upon to do a pastoral visit as a trainee minister was with a woman residing in the long-term care home, and her grandson had died suddenly in chaotic circumstances. She was a complete stranger to me. I did not know her story at
all. So I listened, and I noticed things about the way she spoke about her grandson, her daughter (his mother), her worry about where his soul was. In her story was embedded a deep fear that if her grandson had died before confession of his sins, he was bound
for hell, or at the best, purgatory; and her distress was that she and her daughter would never see him again (but I realized she wasn’t just talking about his physical presence, but eternity.) I looked too. And I saw that there was a crucifix on her wall above the chair where she sat, and that over her bed was a collection of angels surrounding a BVM. I had a private argument with God. “Thanks. My very first pastoral visitation as a UCC minister is to a Roman Catholic! Her theology of death is an ocean away from mine.
And you want me to pray with her?!” BUT I knew enough to remind myself (or perhaps it was the Holy Spirit reminding me):
Her story.
Her life.
Her theology.
Her concerns.
Her spiritual landscape. Not mine.
It became clear – and it often does – that this visit was coming to its natural end. It’s that moment when we make promises to stay connected, and choose, either to pray, or to high tail it out of there! I decided to lean into the praying moment. With some questions, open-ended. I pointed at her BVM, the crucifix, and asked her “Are you a person who prays?”
“Oh yes, she said, but right now I daren’t, because I want God to take him to heaven, and I don’t know if he/God will.”
(In my head, my theology, the answer is “Of Course God will!” But that’s not my role. To impose my theology on her), so I simply said… “Would you mind, if I took a moment to pray, here with you, before I go?”
Visibly relieved, she agreed, and, I prayed a few words, I asked God to take her grandson into the company of heaven. (But I didn’t dress up a sermon in the disguise of prayer), and said some other hopeful pray-y words, until, I swear to this day, that
Blessed Virgin Mary on her wall stared at me… and I started to recite the Hail Mary! And she joined in, “Holy Mary, mother of God, pray for us sinners, now and at the hour of our death. Amen.” She was crying, I cried. And she said, hopeful and determined at last, “ I can ask Mary to pray for him.” And I said, “Yes. You can.”
SUMMARY and TIPS
Prayer then, is the moment in a visit, where you, as a spiritual being having a human experience, find some words to help that other person connect soul and body, connect the trauma with the Healer, conned the despair with God, the source of Hope.
In my story, there was a mixture of extemporary and formulaic prayer. I encourage both.
1. Formulaic prayers.
Be careful. Nowadays, fewer and fewer people have memorized prayers to fall back on. My story was of a devout Catholic. They have lots of prayers, and you may not know them. But if I were to visit a long-time member of a church, I might offer simply to pray the
Lord’s Prayer with them (but I would always try to have that prayer written out. There are places where traditions diverge debts, sins, trespasses, for thine is… etc.) It can also be longer, and more involved. Healing Pathway practitioners, people who are familiar with mediation or yoga practises may be glad to be given the opportunity to “breathe” or to “centre” or to sit in silent prayer.
2. Prayer that is extemporary simply takes elements of what they’ve told you, in the way that they told you, not cleaning it up and making it theologically correct (!), and addressing that to God.
Sick in hospital, No diagnosis. They tell you they’re scared it could be something deadly They tell you they’re lonely. You turn that into a prayer, addressed to God. “God, I pray for Mabel, in this uncertain time, be with her when she feels scared. Let her know you will be with her no matter what. That she is held close to your loving
heart. Amen.”
Someone awaiting surgery. “God, be with Frank as he prepares for his surgery. We pray for his surgeon and the medical team. And we pray too for his recovery. Amen.”
Some people will add their own prayer once you start, and if they do, listen, and wait…and if necessary add a concluding prayer with an Amen.
Always be ready to wait, and always be clear when you’re done. How? “Amen” in a clear tone, followed by “Thank you for letting me pray with you. I will continue to pray (during this crisis).”
Phone and online praying with someone. Even more so, keep your praying short, and if on the phone, don’t leave long pauses, and be explicit if you’re inviting them to add anything. Online: invite them to close their eyes, and close yours too. It feels more ‘prayer like’ and less invasive.
3. Physical/Tangible Prayer: Prayer shawls
a) As a general rule I never touch people with whom I am in pastoral conversation. There’s too much that’s ambiguous about it. The two exceptions I make are a) to share a prayer shawl (if you or your church has a prayer-shawl ministry, this is a great way to literally wrap things up!) Offer the prayer shawl, let them hold or wear it as you pray.
b) At the time of parting, I will offer a hand to theirs, or to a shoulder. As an ordained minister, I may well turn that moment into something that is experienced as a “benediction”. For anyone else, a hand, gently squeezed after your praying is done, can be a real blessing.
AND the LAST STEP: Follow Through.
If your congregation has a prayer list, ask if they would like their name added. Explain the protocol of your church, that the details are not shared, and that if they prefer, no name will be shared aloud.
ASIDE: Congregational prayers are not sideways communications of gossip about private matters!
Always connect with your Minister about people with whom you’ve prayed.
Miscellaneous notes:
Keep an eye on the family caregiver. A verbal acknowledgement could mean the world. Avoid anything that could cause pain or pressure.
Never comment that someone looks exhausted.
Work with your minister to design a simple way for your congregation members to tell the minister about their illness or concerns.
Watch for visitors or regular attendees experiencing a hard time.
Are there tissues handy in your church?
Is there a quiet space available for those who need an escape?
Are the greeters overly exuberant? They might need a reminder to look for hunched shoulders, red eyes, or maybe you want to stand nearby to watch for that. If an out of town son or daughter accompanies someone to church and none of them are smiling, that could be a clue that something’s wrong.
Is someone noticing when regular onsite or online worshippers are missing for several weeks?
Does someone read the Gazette carefully to see if there are obituary notices of grandparents or siblings of your church members?
Is someone tracking death anniversaries to alert the Minister in advance so he/she can send a note?
Using Texting and email for Pastoral Care
Rev. Ellie Hummel, Multidisciplinary Chaplain, Mount Allison University
The main focus of pastoral care, whether in person, by phone, by text, email or social media is to be present and allow room for the Spirit. The person is a child of God.
Use the right tools – and be sure it is something you are comfortable with. Be aware of what is public and what is not.
Young people do not use email, nor do they check voice mail. Seniors often use texting and private messages. Ask the person which platform they prefer to use.
Passive use of social media:
- pay attention if you see someone posting sad messages. Observe trends and any radical changes, and send a private message to check in.
Active use of the various platforms:
- confirm if the communications platform is private by asking directly: ‘Can I text you there?’ Be aware that some people have shared email accounts.
- manage expectations. If you will only be available work days between certain times, be clear. You don’t need to be available 24/7. Say ‘I usually respond within a day’.
- Take your time when you are writing a reply. Practise the Pause. Reread your message before sending it. Watch out for autocorrect and spell check.
- Be careful with emojis. Poop emoji is not a cookie!
- Heart emojis mean different things to different people. Better to avoid them.
- Ensure that nothing you write could be misconstrued.
- Anecdote: in the US there was a legal contract and the receiver used a thumbs up emoji to confirm receipt but did not sign the contract. The court ruled that the thumbs up meant an agreement to the terms of the contract.
- Remember there is lots of room for misinterpretation and you don’t want to sound like you are giving advice.
- Avoid asking a lot of questions. Create a circle of love without making the person tell their story again.
Using social media tools to connect with people and build relationship of trust:
- Thinking of you
- Holding you in prayer
- Sending good thoughts
- Let me know if you want to chat some more
- If you need to talk, I’m here
- Would you like to meet to chat?
- Would it be helpful to video chat together?
- This sounds like something that needs a larger conversation
- Hmmm. That must be hard.
- I hear you.
- It sounds like this was a hard day.
In traumatic times, the person does not always feel like talking – it takes too much energy. Be open to further chat when they feel ready.
Be gentle with yourself. You don’t have to do pastoral care electronically if you are not comfortable.
Using texting and private social media messaging platforms are useful for checking in on someone and can reduce loneliness and isolation. Messages don’t have to be long. The person will know you are thinking about them.
Shared experiences:
- 2 long-time friends who live alone but in different geographic areas text each other each morning to say hi or to share what’s on their heart.
- Texting is often easier on seniors than email. Voice to text or using iPad with bigger font can be helpful.
- Texting with someone in hospital means no one else can hear what they are sharing.
Additional note shared by a participant after the session:
- Avoid saying anything on Facebook about a death until the family has shared something publicly. It’s their news, no matter how sad you might be.
Comforting the Mourner
Corrie Sirota M.S.W., P.S.W. OTSTCFQ, OPQ
Grief, Loss and Bereavement Specialist - Counseling & Psychotherapy
Clinical Director, Myra's Kids Foundation www.myraskids.ca
[email protected]
Author of "Someone Died...Now What? A Personal and Professional
Perspective on Coping With Grief and Loss" available on amazon.com
There are 72 euphemisms for ‘died’. People are uncomfortable talking about death.
People grieve differently, the stages of grief are not linear, grief will not go away if you ignore it, children definitely grieve, but in different ways, you don’t know exactly how someone feels, there is no shame in seeking counselling.
Death ends a life, not the relationship. Listen, provide support in ways that are relevant to the person, use the name of the person who died, honour the deceased by recognizing death anniversaries, birthdays, etc.
Be aware that there may be complications to the grief and secondary losses such financial impact, where to live, social fall-out, etc.
Click here for Corrie’s TEDx Laval presentation: Loss and Found: Creating New Normals After Someone You Love Dies:
https://youtu.be/PQ27tYEb74Y
And here is a link to her McGill cares webcast: https://www.youtube.com/watch?v=oATZ9cMVGXs
Pastoral Care Challenges as a Giver and as a Receiver
Paul Clarke
Paul Clarke has been a care receiver and a care provider over the years. He shared some personal stories to illustrate pastoral care, including potential pitfalls of good intentions.
- Community oten responds with food and the care receiver ends up with a freezer full of food but nothing for dinner. A nice gesture can become overwhelming, creating a logistical problem when they have to give it away.
- It's difficult to know how to say no so as a Pastoral Care Team member, anticipate when enough is enough.
- One person called ahead and brought a complete meal: pasta sauce, a box of pasta, a salad, a baguette and even a bottle of wine. Paul never forgot that very thoughtful, caring gift.
- People made well-intended but poorly thought out remarks; a lot has changed in awareness since the late 1980s but it’s very important to choose words carefully to avoid hurting the care receivers.
- Offer practical, logistical, and caring help, such as babysitting.
- ‘Call me if I can help’ is not helpful.
- Encourage the care receiver to tell you exactly what would be helpful to them.
- Be careful when poorly thought out comments can upset someone, making them feel pitied.
- Multiple losses or challenges do not identify a family.
- A community can sometimes know too much; confidentiality and discretion are essential in pastoral care.
- As a pastoral care team member, always recommend that people reach out to CLSC to get a file created so that when they need additional assistance, it’s easier. Don’t wait for a crisis!
- Know what outside resources are available and offer information about them.
When offering pastoral care, it's often very similar to being a good neighbour, part of a caring community,
- investing time in the friendship
- answering calls for assistance (anecdote: friends using wheelchairs who needed help puicking up dropped items like the remote
- sharing meals together – including BBQs, something they might have loved doing in the past but can no longer manage
- playing cards on a quiet afternoon.
- driving them to appointments or a wedding, taking them for meals, picking up groceries, setting out their garden furniture, planting their garden with them, offering to call family members when the need arises.
- keeping an eye open for needs that won’t be requested
- It’s important to ask if the care receiver wants to do something on their own, rather than assuming they need help.
- One line Paul uses regularly when it came to medical or financial info: “I have an indelicate question; feel free to tell me to mind my own business.” With a relationship built on trust, the care receiver will share only what they feel comfortable with.
- Pastoral care is important when someone is out of work. offer to take the person for coffee, or to a pub, to give them space to talk.
Understanding Cultural Context in Our New Demographic
Paul Clarke
In 2013 Paul started working at Action Refugiés Montreal, a small NGO that accompanies refugeed people. Their model is empowerment vs charity.
Things to consider when offering pastoral care or caring community friendship to people who have moved from other countries:
- Some societies do not talk things out like we do; they have different basis for health, mental health, may be more family oriented.
- Small things can be triggers. Family members lost due to violence, lived hardships on way to Canada. Be aware, be sensitive, listen without judgement or platitudes.
- Be respectful about issues such as physical touch, embracing. Not all cultures are the same.
- Be aware of figures of speech that might be unfamiliar or which could be misinterpreted.
- Most new arrivals don’t want to bother others. Not aware of resources available.
- Not all new arrivals want to meet members of their community: overseas conflicts might be brought here, so some want nothing to do with their community. It’s important to be aware of that dynamic.
- There can be a strong distrust of authorities, including doctors.
- It’s okay to ask about their customs. In the case of a death and the person cannot return to their country of origin, ask ‘what would you be doing if you were there?’; ‘how does it work there?’ Are there ways you can help replicate that – if that’s what the person wants?
Prayer in visiting/care settings
Rev. Dr. Elisabeth Jones, Cedar Park United Church
Prayer is one thing we all need. Because we’re spiritual beings having a human experience. Mortality undoes us.
Ours, or a loved one’s. Illness – physical, mental, catastrophe, unemployment, not enough money, addictions, gender issues… we experience all of these not just in our matter, our cells, our physical assembly, but in our souls, our beings. We know that prayer takes us to holy ground/space. We tread carefully, and consciously. And it’s a hairbreadth line between careful, conscious prayer with and for another, and self-conscious stumbling (or at least feeling that way! But it’s really worth trying to become a person who can pray with and for (not at or about) someone. So I want to say it IS an essential part of the work of a pastoral care team. And it
should never be left to the Minister to do alone.
Because stories are easier to retain in memory. I’m going to make 5 points about this topic, but to frame them within a story, drawn from my experience.
STORY
The first time I was called upon to do a pastoral visit as a trainee minister was with a woman residing in the long-term care home, and her grandson had died suddenly in chaotic circumstances. She was a complete stranger to me. I did not know her story at
all. So I listened, and I noticed things about the way she spoke about her grandson, her daughter (his mother), her worry about where his soul was. In her story was embedded a deep fear that if her grandson had died before confession of his sins, he was bound
for hell, or at the best, purgatory; and her distress was that she and her daughter would never see him again (but I realized she wasn’t just talking about his physical presence, but eternity.) I looked too. And I saw that there was a crucifix on her wall above the chair where she sat, and that over her bed was a collection of angels surrounding a BVM. I had a private argument with God. “Thanks. My very first pastoral visitation as a UCC minister is to a Roman Catholic! Her theology of death is an ocean away from mine.
And you want me to pray with her?!” BUT I knew enough to remind myself (or perhaps it was the Holy Spirit reminding me):
Her story.
Her life.
Her theology.
Her concerns.
Her spiritual landscape. Not mine.
It became clear – and it often does – that this visit was coming to its natural end. It’s that moment when we make promises to stay connected, and choose, either to pray, or to high tail it out of there! I decided to lean into the praying moment. With some questions, open-ended. I pointed at her BVM, the crucifix, and asked her “Are you a person who prays?”
“Oh yes, she said, but right now I daren’t, because I want God to take him to heaven, and I don’t know if he/God will.”
(In my head, my theology, the answer is “Of Course God will!” But that’s not my role. To impose my theology on her), so I simply said… “Would you mind, if I took a moment to pray, here with you, before I go?”
Visibly relieved, she agreed, and, I prayed a few words, I asked God to take her grandson into the company of heaven. (But I didn’t dress up a sermon in the disguise of prayer), and said some other hopeful pray-y words, until, I swear to this day, that
Blessed Virgin Mary on her wall stared at me… and I started to recite the Hail Mary! And she joined in, “Holy Mary, mother of God, pray for us sinners, now and at the hour of our death. Amen.” She was crying, I cried. And she said, hopeful and determined at last, “ I can ask Mary to pray for him.” And I said, “Yes. You can.”
SUMMARY and TIPS
Prayer then, is the moment in a visit, where you, as a spiritual being having a human experience, find some words to help that other person connect soul and body, connect the trauma with the Healer, conned the despair with God, the source of Hope.
In my story, there was a mixture of extemporary and formulaic prayer. I encourage both.
1. Formulaic prayers.
Be careful. Nowadays, fewer and fewer people have memorized prayers to fall back on. My story was of a devout Catholic. They have lots of prayers, and you may not know them. But if I were to visit a long-time member of a church, I might offer simply to pray the
Lord’s Prayer with them (but I would always try to have that prayer written out. There are places where traditions diverge debts, sins, trespasses, for thine is… etc.) It can also be longer, and more involved. Healing Pathway practitioners, people who are familiar with mediation or yoga practises may be glad to be given the opportunity to “breathe” or to “centre” or to sit in silent prayer.
2. Prayer that is extemporary simply takes elements of what they’ve told you, in the way that they told you, not cleaning it up and making it theologically correct (!), and addressing that to God.
Sick in hospital, No diagnosis. They tell you they’re scared it could be something deadly They tell you they’re lonely. You turn that into a prayer, addressed to God. “God, I pray for Mabel, in this uncertain time, be with her when she feels scared. Let her know you will be with her no matter what. That she is held close to your loving
heart. Amen.”
Someone awaiting surgery. “God, be with Frank as he prepares for his surgery. We pray for his surgeon and the medical team. And we pray too for his recovery. Amen.”
Some people will add their own prayer once you start, and if they do, listen, and wait…and if necessary add a concluding prayer with an Amen.
Always be ready to wait, and always be clear when you’re done. How? “Amen” in a clear tone, followed by “Thank you for letting me pray with you. I will continue to pray (during this crisis).”
Phone and online praying with someone. Even more so, keep your praying short, and if on the phone, don’t leave long pauses, and be explicit if you’re inviting them to add anything. Online: invite them to close their eyes, and close yours too. It feels more ‘prayer like’ and less invasive.
3. Physical/Tangible Prayer: Prayer shawls
a) As a general rule I never touch people with whom I am in pastoral conversation. There’s too much that’s ambiguous about it. The two exceptions I make are a) to share a prayer shawl (if you or your church has a prayer-shawl ministry, this is a great way to literally wrap things up!) Offer the prayer shawl, let them hold or wear it as you pray.
b) At the time of parting, I will offer a hand to theirs, or to a shoulder. As an ordained minister, I may well turn that moment into something that is experienced as a “benediction”. For anyone else, a hand, gently squeezed after your praying is done, can be a real blessing.
AND the LAST STEP: Follow Through.
If your congregation has a prayer list, ask if they would like their name added. Explain the protocol of your church, that the details are not shared, and that if they prefer, no name will be shared aloud.
ASIDE: Congregational prayers are not sideways communications of gossip about private matters!
Always connect with your Minister about people with whom you’ve prayed.
